Bacteriophage.me

Bacteriophage.me
Introduction
to Bacteriophages
Bacteriophages (or phages) are viruses that infect and kill bacteria. First discovered in the early 20th century, they are being reconsidered today due to the rise of antibiotic-resistant bacteria. Phage therapy is gaining attention as an alternative treatment in clinical settings, especially where traditional antibiotics fail. Phages are highly specific, only targeting the bacteria they are designed for, making them an exciting solution in the fight against antimicrobial resistance.
Clinical Applications
Phage therapy has shown success in treating infections resistant to antibiotics, such as those caused by Staphylococcus aureus and Pseudomonas aeruginosa. Current clinical trials are testing the efficacy of phage cocktails and engineered phages in addressing chronic infections where antibiotics have failed. One of the most promising areas is CRISPR-engineered phages, which use gene-editing tools to enhance their bacterial targeting ability.
Several case studies have demonstrated the potential of phage therapy in real-world scenarios. For example, phage therapy was used successfully to treat a life-threatening Staphylococcus infection at UC San Diego in 2017. Ongoing trials aim to expand these treatments to more resistant bacterial infections, offering a targeted solution for difficult-to-treat cases.
Mechanism of Action
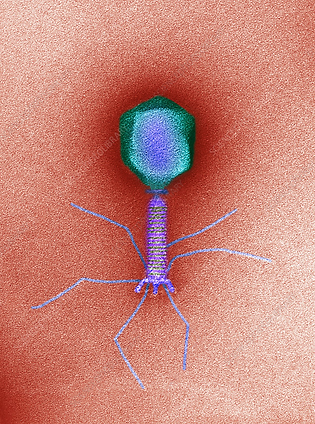
Phages work by infecting bacteria, injecting their genetic material into the host cell, and using the bacterial machinery to replicate. After replication, they cause the bacterial cell to burst (lyse), releasing new phages to infect more bacteria. Phages are categorized into two main types: lytic phages, which destroy the bacteria immediately, and lysogenic phages, which integrate their DNA into the host cell and replicate with it until triggered to enter the lytic phase.
Phages' ability to specifically target bacteria without harming human cells or beneficial microbiota makes them a promising tool for treating infections. This specificity is an advantage over broad-spectrum antibiotics, which can kill beneficial bacteria and lead to further health issues.
Phage Therapy in Practice
Phage therapy is administered in several ways, including oral, topical, and intravenous methods. The delivery method depends on the infection site and type of bacteria being targeted. In clinical settings, phage therapy can be used as an adjunct to antibiotics or as a standalone treatment for drug-resistant infections. Safety is a top priority in phage therapy, with strict protocols ensuring that the selected phages are specific to the bacterial infection. Hospitals and clinical trials currently offer phage therapy to patients with severe infections that do not respond to antibiotics, such as in cases of chronic wounds, respiratory infections, or sepsis.


Research and Future Directions
The future of phage therapy looks promising, with ongoing research into synthetic phages and phage cocktails. Synthetic biology allows researchers to design phages that can target specific bacteria more effectively, opening the door to custom treatments for individual patients. This aligns with the broader trend of personalized medicine, where treatments are tailored to a patient’s specific infection profile.
Upcoming clinical trials in 2024 are exploring the use of phages in combination with antibiotics to improve treatment efficacy. These trials could pave the way for more widespread use of phage therapy in clinical practice, particularly in hospitals dealing with high rates of antimicrobial resistance.